Avicenna Menopause Clinic
Introduction
At Avicenna Menopause Clinic (AMC) we have a deep understanding of the challenges faced by women during the menopause transition and beyond.
Our menopause specialists combine extensive experience with a compassionate approach and are dedicated to enhancing the overall well-being and future health of perimenopausal and menopausal women of all ages.
We integrate the latest evidence-based treatments with individualized, holistic programs to suit your needs.
About the service
Initial consultation:
Your first consultation at Avicenna Menopause Clinic, will allow plenty of time for you to feel listened to, this is usually around 45 minutes. We will discuss your symptoms and your main concerns, working out a treatment plan to best suit you as an individual. You can be seen face-to-face at our clinic, or via a secure video link.
Prescriptions:
Medication will be prescribed as a private prescription and
can be emailed to the pharmacy of your choice. If you need more time to consider your treatment plan, you have up to 3 months to let us know.

Communication after your appointment:
Your treatment plan and detailed clinical letter will be emailed out to you, usually within a few days of your appointment.
Each initial consultation includes one email enquiry if there was anything you forgot to ask during the consultation, or if you have any questions once you have started treatment. This is intended to be used as a quick query and does not replace your follow up appointment.
3 months after your initial consultation:
Typically, 3 months after your initial consultation, you will have been advised to book a follow up appointment. This is important in order for us to ensure we have found the right treatment and dose for you to optimise alleviation of your symptoms and your ongoing health. At this point we may make adjustments to your treatment plan.
6-12 months after your follow up appointment:
Your hormone requirements may continue to change during your lifetime. There may also be new treatments available or new guidelines for us to discuss. We therefore recommend our patients are seen at least annually in line with the British Menopause Society practice standards.
If you have been prescribed testosterone, we will need to organise an annual blood tests prior to your follow up.
We are always here to help, should you wish to be seen sooner than planned.
Meet our Clinician

Lindsey Lester
Prescribing Menopause Specialist
Our esteemed menopause specialist brings extensive experience and a compassionate approach to our GP practice. She is dedicated to enhancing the overall well-being and future health of perimenopausal and menopausal women of all ages.
Appointment types and prices
Please click the appointment type for more information and to book an appointment.
1.AMC Initial Consultation (£185)
2. AMC Follow-up Consultation (£135)
3.Testosterone Initial Assessment and HRT Review (£185)
4.Genitourinary Symptoms Only (£150)
5.Interim Telephone Call (£65)
6.Additional Medical Letters (£50)
7.Prescription Fee (£35)
Frequently Asked Questions (FAQs)
What is menopause?
Menopause can be split into three stages:
1. Perimenopause
Perimenopause is the time in a woman’s life when hormone levels start to fluctuate due to lessening ovarian function. Periods often change, becoming lighter or heavier, closer together or further apart. You may experience symptoms related to the fluctuations and these can often be more severe than during menopause itself. Perimenopause can last for up to 10 years. It is sometimes described as ‘reverse puberty’.
- Menopause
Menopause is said to have occurred when you have had 12 consecutive months without a period.
3.Postmenopause
The time in your life after menopause has occurred. Symptoms may continue due to the continuing lack of hormones.
What are the symptoms of menopause?
There are many symptoms that may be experienced around the menopausal transition including physical, psychological and genitourinary symptoms. Symptoms can be as individual as people and not everyone gets the most well talked about hot flushes and sweats. This may make it more difficult to know if you are having symptoms or not. Symptoms may also change over time and new ones develop.
Physical symptoms include:
Hot flushes, sweats, chills, heart palpitations, headache/migraine, sleep disturbances, joint pain, weight gain, hair changes, dry skin, loss of libido, dry eye.
Psychological symptoms include:
Low mood, anxiety, mood swings, irritability, memory problems, difficulty concentrating, loss of interest, crying spells, brain fog, loss of self-esteem.
Genitourinary symptoms of menopause (GSM):
These are extremely common and can continue for the rest of your life if left untreated.
Vaginal dryness, pain or discomfort during intercourse, urinary frequency, urinary urgency, urinary tract infections.
At what age does menopause occur?
In the UK, the average age of menopause is 51, however some women will experience it earlier or later.
On average, hormones can start to change from age 35 and often symptoms can be noticed from late 30’s-early 50’s.
Menopause under the age of 40 is known as premature ovarian insufficiency. This affects 1 in 100 women under 40 ,1 in 1000 under 30 and 1 in 10,000 under the age of 20.
The permanent cessation of periods between the age of 40 and 45 is known as early menopause.
Surgical menopause occurs when the ovaries are surgically removed and menopause will be very sudden.
Medical menopause may occur due to treatment such as radiotherapy, chemotherapy or treatment for some medical conditions.
It is vital that women experiencing menopause before the average age of 51, replace their hormones , except in very particular circumstances.
Do I need a blood test to confirm menopause?
The NICE guideline (National Institute for Clinical Excellence) states that perimenopause should be diagnosed on symptoms alone for healthy women over the age of 45.
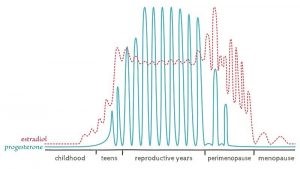
Because hormone levels fluctuate so erratically during perimenopause, blood tests are often unreliable and only represent a snapshot at the particular time the blood was taken. It can sometimes be helpful to use blood testing for other reasons.
Women under the age of 40, who have not had a period for four months or longer, or who have symptoms suggestive of oestrogen deficiency, may be advised to have two blood tests, taken 4-6 weeks apart to aid diagnosis.
See the diagram below, which demonstrates how vast the hormonal fluctuations can be at perimenopause.
Do I need a referral letter from my GP to be seen at the clinic?
No, most women will self-refer. If you have any relevant medical or gynaecological letters, it may be helpful to send a copy prior to your appointment or bring it along to your appointment.
How long will my symptoms last?
We are all individual and some women will have symptoms for a few months perhaps, while other will continue having symptoms for the rest of their lives.
On average symptoms last between 4-10 years. Some symptoms can come and go, and others can become more problematic over time.
Why should I consider treating my symptoms?
Oestrogen plays an important role in many areas of the body, helping in particular to maintain bone, heart, brain and pelvic health. It is thought by some scientists, that the severity of symptoms may have an impact on our future health and the more effectively the symptoms are treated, the better the outcome.
Bone: Research has shown that oestrogen can help to maintain bone strength, preventing osteoporosis and fragility fractures. One in 2 women over the age of 50 will sustain a fracture during their lifetime, compared to one in 5 men. HRT is licensed to prevent osteoporosis.
Heart: Oestrogen is known to have a positive effect on blood vessels and starting treatment with HRT can have a protective effect on heart health, provided treatment is started within 10 years of the final period.
Lower levels of oestrogen seen during menopause, can lead to build up of plaque and hence narrowing of arteries which could increase the risk of heart attacks or strokes.
Cholesterol: Oestrogen helps to control cholesterol levels, reducing the risk of plaque building up inside the artery walls.
Diabetes: Research has shown that oestrogen helps to control blood glucose levels and can therefore be helpful in the prevention of type 2 diabetes.
Brain: New research shows the changes that occur at menopause in the brain are due to the lack of oestrogen. Almost two thirds of Alzheimer’s patients are post-menopausal women. It is thought the sooner HRT is initiated, the better and it should be started under the age of 65 for brain health.
How long does it take for HRT to work?
It can vary between individuals. Some women begin to feel improvements quite quickly, whereas for others, it can take three months to feel the full effects. It is worth persevering with any treatment for 3 months and following the recommendations on your treatment plan. For some women, it may be necessary to try a few options before finding the one that suits them best.
Are there any side effects of HRT?
As with all medication, some women will notice side effects initially, but often these improve over the first 3-6 months once your body has had time to adjust. The most common side effects, should they occur, are bleeding, bloating and breast tenderness.
If any of these occur and have not settled by the time you have your follow up consultation, we may make adjustments to your HRT.
Will I bleed on HRT?
It is very common for women to have irregular or sometimes heavy bleeding when they start HRT or after adjusting their dose of oestrogen. It is normal for this to settle after 3-6 months and adjustments may be made at your follow up appointment.
You should speak to your menopause clinician or GP if bleeding is particularly heavy or is worrying you.
What are the risks and benefits of HRT?
Although there have been concerns raised about the safety of HRT over the years, more recently published research shows that it remains the most effective solution for the relief of menopausal symptoms and is also effective for the prevention of future health risks such as osteoporosis and cardiovascular disease. There are other potential benefits such as improved cholesterol profile, improved blood glucose control and maintaining brain health. For most women, the benefits outweigh any risks when HRT is initiated within 10 years of the last period or before the age of 60. Starting HRT after the age of 60, there will still be benefits in terms of quality of life and bone health, but any further benefit is less clear.
Benefits continue, for as long as HRT is used and NICE guidelines state that there is no arbitrary age limit.
It is important to distinguish between the more natural types (body identical) of hormones that are now available, compared to the older, synthetic types that most of the negatively publicised data were referring to.
There are studies which show that body identical HRT containing micronised progesterone and estradiol, do not increase the risk of breast cancer for at least the first five years of use in women above the age of 51. For women younger than 51, there is no increased risk. Importantly, the studies show that there is no increased risk of death from breast cancer for women taking HRT.
There remains widespread confusion and uncertainty amongst both doctors and women taking HRT. Many doctors simply stopped prescribing it when the Women’s Health Initiative (WHI) study was published in 2002, and the numbers of women taking it dropped by 66%. It should be noted that breast cancer rates have continued to increase, despite the drastic decrease in HRT use.
Oral oestrogen and some synthetic progestogens have been shown to have a small increased risk of blood clot, however the research has shown that there is no increased risk when using transdermal oestrogen (through the skin).
For more information relating to the risks and benefits please read the following factsheet: https://www.womens-health-concern.org/wp-content/uploads/2022/12/11-WHC-FACTSHEET-HRT-BenefitsRisks-NOV2022-B.pdf
What is body identical HRT?
Body identical HRT refers to hormones derived from natural sources whose structure is the same as our bodies naturally produced hormones. They therefore fit our receptors more effectively than synthetically manufactured hormone analogues. We only use regulated, licensed products in our clinic, and these are the safest type of HRT with the lowest incidence of side effects.
The British Menopause Society does not support the use of compounded ‘Bioidentical hormones’, as they are custom made in manufacturing pharmacies without the rigorous quality assurance that standard prescription medicines are subject to.
Is HRT the only available treatment?
No, but it is the most likely to help with the full range of symptoms as it is replacing the hormones that your body is no longer making and treating the root cause. The doses are actually very small, and we just use enough to get you feeling like yourself again.
For those that don’t like the idea of hormones, there are alternatives, but it is important to make sure you understand the risks and benefits of all treatments before making a decision. You may not have been given the correct information previously.
Not all HRT is equal, at Avicenna Menopause Clinic, we will prescribe the most suitable and safest options.
Am I too old to start HRT? How about vaginal oestrogen?
Not necessarily. We know that the cardiovascular benefits of HRT occur when women start treatment before the age of 60 or within 10 years of their menopause. However, it is always important to consider the individual and if symptoms are seriously affecting quality of life, there are still benefits to be gained. Your personal medical history will also be an important consideration.
The British Menopause Society advises that any decision should be made on an individualised basis after discussing the risks and benefits.
There are very few instances where vaginal oestrogen would not be suitable, so this is always an option that can be discussed. Vaginal oestrogen can be really effective for both vaginal dryness and urinary symptoms such as urgency or incontinence. There are a few options to try and if effective, treatment should be continued indefinitely.
I have been told I can’t have HRT; would other treatments be safe for me?
First we will make sure you have been given the correct advice. There are a number of alternatives both prescribable and complementary therapies which can be used alongside lifestyle optimisation that can be effective.
Common misconceptions are that HRT should be avoided in migraine, blood clotting disorders, history of stroke or previous blood clot, however it’s the type of HRT that matters.
Do you prescribe Veoza, the new non hormonal drug for hot flushes/night sweats?
Yes, we do, as long as it is suitable.
Veoza (drug name Fezolinetant) has recently been launched in the UK as a non-hormonal treatment option for moderate to severe vasomotor symptoms (hot flushes and night sweats). The active ingredient in Veoza is called Fezolinetant. This is a neurokinin 3 antagonist that works by blocking the neurokinin 3 receptors in the brain that play an important role in the regulation of body temperature – so it works to block the source of the hot flush. Prior to menopause, oestrogen helps to keep things nicely balanced.
Veoza may be suitable to use in some conditions where you have been advised not to take HRT. It is important to note that it has not been studied in women who have been diagnosed with breast or other cancers, but research is currently being carried out. A discussion with a menopause specialist or oncologist is important when deciding whether Veoza is suitable for you if you have had cancer.
I’ve heard people use patches or gel; can I take HRT tablets?
Some oral types of HRT have been shown to slightly increase the risk of blood clot or stroke, it is therefore considered safer in most cases to use ‘transdermal’ (through the skin) oestrogen in the form of patch, gel or spray with oral capsules of micronised progesterone. In women with no risk factors for blood clot or stroke, oral HRT may be considered if this is the preferred option.
It is still possible to take ‘body identical’ hormones which are more breast friendly, even in oral form.
It should be noted that oral oestrogen may reduce the level of circulating testosterone and therefore can reduce libido.
Why do some women use testosterone?
Testosterone is an important hormone in the female body and is made in the ovaries, adrenal glands and brain. Levels of testosterone decline at perimenopause and menopause which can lead to a variety of symptoms such as low energy/motivation, lack of sex drive (libido) and brain fog.
Replacing testosterone can work to improve these symptoms as well as bone and muscle strength. It can take several months of using testosterone before a benefit is noticed.
Are there any side effects of testosterone?
Side effects are very unlikely as long as the blood levels are kept in the correct range. The most common side effect is increased body hair at the site of application, and this can be minimised by using several different areas of application.
Studies looking at the effects of testosterone in women are currently limited to a 2–3-year period but these do suggest a good safety profile. They demonstrate that testosterone:
1. Is safe when prescribed as a preparation absorbed through the skin at low doses
2. Causes no increase in blood pressure
3. Has no adverse cardiovascular effects
4. Has no impact on breast cancer risk
5. Does not stimulate the womb lining
Can I get a prescription for testosterone from you?
If you have already been established on HRT but still have symptoms that indicate low testosterone such as low libido, low energy/motivation, then we can discuss a trial of testosterone.
This will need to be monitored with blood testing to make sure you are absorbing it well, but remain within the female range. If you prefer, we can check your blood levels prior to treatment. We normally test your blood after 3 months and make adjustments, if necessary, at a follow up appointment. Once we are happy with your results, an annual review with blood test is required to continue with your prescription.
How do I receive the results to my blood tests?
We normally request that blood tests be taken prior to a follow up appointment in time for the results to be available to discuss in person. For any other blood test result, your clinician will review and comment on them via email.
How often will I need to be seen?
After the initial consultation, we would like to see you again after 3 months to see if you need any adjustments to your treatment plan. We may have discussed blood tests at your initial appointment, and these should be arranged around 7-10 days prior to the follow up if possible. The follow up is recommended in order to give you the best possible care and to ensure your treatment has been optimised and is suitable for you to continue.
Once you are happy with your symptom control, you can choose to be seen every 6-12 months as you prefer. It is important that women taking HRT are seen at least annually.
Are there any additional costs?
Unlike some other clinics, we do not charge an administration fee for any prescriptions created within the appointment.
We may recommend blood testing and the price will depend on the types of tests ordered.
The prescriptions will be private as we are a private clinic, and therefore the items will be charged for according to their cost by the pharmacy of your choice.
Do you tell my GP about my treatment?
You will receive a letter detailing your treatment and it is up to you if you wish to share it or not. Of course, if you do see your GP, it is advisable to let them know, as it may be relevant.
fURTHER INFORMATION & TOPICS THAT MAY HAVE BEEN DISCUSSED IN YOUR CONSULTATION
Bleeding after menopause (post-menopausal bleeding)
PI Post-Menopausal Bleeding PMB poster (womens-health-concern.org)
Brain health
https://foodforthebrain.org/campaigns/alzheimers-prevention/omega-3-and-b-vitamins/
https://news.weill.cornell.edu/news/2024/06/scans-show-brains-estrogen-activity-changes-during-menopause#:~:text=Credit%3A%20Mosconi%20lab.,researchers%20at%20Weill%20Cornell%20Medicine.
Breasts -How to check them
https://coppafeel.org/wp-content/uploads/2023/05/CoppaFeel-chest-checking-leaflet-2023.pdf
Bone health and calcium calculator
https://theros.org.uk/information-and-support/bone-health/nutrition-for-bones/calcium/
Bone health and exercise
https://theros.org.uk/information-and-support/bone-health/exercise-for-bones/?gad_source=1&gclid=CjwKCAjw65-zBhBkEiwAjrqRMD-ZJXK4Mh0FqHYmQm9n7SLK3iy2929tzuOv_ISQXgvuSLM_GTsoTRoCh4YQAvD_BwE
Bone Health –Osteoporosis
19-WHC-FACTSHEET-Osteoporosis-Bone-NOV2022-B.pdf (womens-health-concern.org)
Breast cancer risk factors
01-WHC-FACTSHEET-BreastCancer-NOV2022-C.pdf (womens-health-concern.org)
Cholesterol – how to lower it through diet
https://www.bhf.org.uk/informationsupport/risk-factors/high-cholesterol/five-top-questions-about-lowering-cholesterol
Cognitive Behavioural Therapy Factsheet:
https://www.womens-health-concern.org/wp-content/uploads/2023/02/02-WHC-FACTSHEET-CBT-WOMEN-FEB-2023-A.pdf
Complimentary and alternative therapies
03-WHC-FACTSHEET-Complementary-And-Alternative-Therapies-NOV2023-C.pdf (womens-health-concern.org)
Contraception for older women
04-WHC-FACTSHEET-ContraceptionForTheOlderWoman-NOV22-B.pdf (womens-health-concern.org)
Diet and menopause
https://www.bda.uk.com/resource/menopause-diet.html
Diet- The Mediterranean Diet
https://www.uhcw.nhs.uk/download/clientfiles/files/Patient%20Information%20Leaflets/Clinical%20Support%20Services/Dietetics/Mediterranean%20diet.pdf
Emotional wellness in menopause
30-WHC-FACTSHEET-Emotional-wellness-in-menopause-JUNE2023-A.pdf (womens-health-concern.org)
Endometriosis
Endometriosis – Women’s Health Concern (womens-health-concern.org)
Environmental toxins
The Dirty Dozen – Pesticide Action Network UK (pan-uk.org)
Yuka – The Mobile App That Scans Your Products
Epilepsy and menopause
32-WHC-FACTSHEET-Epilepsy-the-menopause-and-HRT-JAN2024-A.pdf (womens-health-concern.org)
Exercise and menopause
29-WHC-FACTSHEET-Exercise-in-menopause-JUNE2023-A.pdf (womens-health-concern.org)
Fibroids
07-WHC-FACTSHEET-Fibroids-NOV2022-A.pdf (womens-health-concern.org)
Glycaemic index of food
https://www.bda.uk.com/resource/glycaemic-index.html
Hair loss
16-WHC-FACTSHEET-MenopausalHairLoss-NOV2022-B.pdf (womens-health-concern.org)
Insomnia and menopause
17-WHC-FACTSHEET-Menopause-and-insomnia-NOV2022-B.pdf (womens-health-concern.org)
Sleepio – Digital Sleep-Improvement help (pathfields.nhs.uk)
Menopause- Understanding menopause
MEN0921351544-005_Menopause-Support-Booklet-5-3.pdf (womens-health-concern.org)
Migraine and menopause
18-WHC-FACTSHEET-Migraine-and-HRT-NOV2023-B.pdf (womens-health-concern.org)
National Migraine Centre – specialist migraine clinic
Polyps in the uterus
24-WHC-FACTSHEET-Uterine-Polyps-NOV2022-B.pdf (womens-health-concern.org)
Premature Ovarian Insufficiency (POI)
What is POI (daisynetwork.org)
Prolapse
21-WHC-FACTSHEET-Prolapse-NOV2022-B.pdf (womens-health-concern.org)
Urogenital symptoms
23-WHC-FACTSHEET-UrogenitalProblems-OCT2023-B.pdf (womens-health-concern.org)
Home Page – Squeezy (squeezyapp.com)
Bladder_Training_RV2.pdf (yourpelvicfloor.org)
Vaginal dryness
25-WHC-FACTSHEET-VaginalDryness-OCT2023-B.pdf (womens-health-concern.org)
Weight gain and menopause
31-WHC-FACTSHEET-Weight-Gain-and-menopause-JUNE2023-A.pdf (womens-health-concern.org)
Supplements to consider
Although some supplements lack hard evidence due to a lack of research and funding, there are some vitamins/minerals that become depleted as we age but have important functions.
Vitamin D3+K2 (For bone health and immunity). Recommended to be taken at least throughout the winter months September-April or continuously if you do not get much sun on your skin. The NHS recommend 400-1000IU daily, but many women are still deficient at menopause. A blood test will allow us to check your requirements.
Magnesium– Magnesium is an important mineral for the body, acting in over 300 different enzyme reactions that regulate various processes such as muscle and nerve function, blood sugar control, and blood pressure regulation.
It has been linked to everything from improved sleep, cognitive function and is involved in hormone metabolism/detoxification alongside B vitamins.
Magnesium rich foods include green leafy vegetables like spinach, avocado, nuts, seeds, legumes and pulses, whole grain foods, tofu and fish such as salmon and mackerel. It is thought most adults don’t get enough in their diet and a supplement containing 300-400mg can be helpful. Please check suitability if you are taking medication from your GP.
There are different types of magnesium depending on your symptoms: –
Magnesium glycinate- perimenopausal symptoms, anxiety, insomnia, calming the nervous system.
Magnesium sulphate (Epsom salt baths)- detoxification, muscle/joint pain, relaxation
Magnesium malate- fibromyalgia, muscle pain.
Magnesium citrate- digestion and constipation.
Magnesium threonate- cognitive /brain health, mood disorders
Magnesium taurate- heart health, blood sugar balance.
Vitamin B complex containing methylated B12, B6, folate rather than folic acid and usually B1, B2, B3, B5. These work well with magnesium in hormone metabolism.
Omega 3 fish oil- people from countries who eat a diet rich in omega 3’s have been shown to have a lower risk of heart disease than the UK population. Omega 3 fatty acids are also considered the most important nutrient for brain function and mood disorders even having links to reducing the risk of Alzheimer’s.
https://www.bda.uk.com/resource/omega-3.html
https://foodforthebrain.org/campaigns/alzheimers-prevention/omega-3-and-b-vitamins/
.